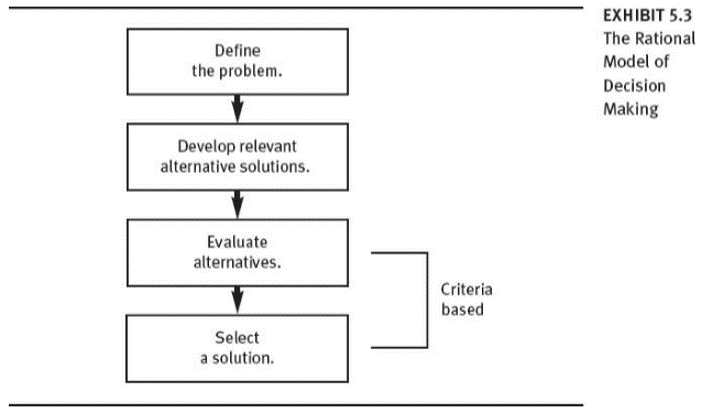
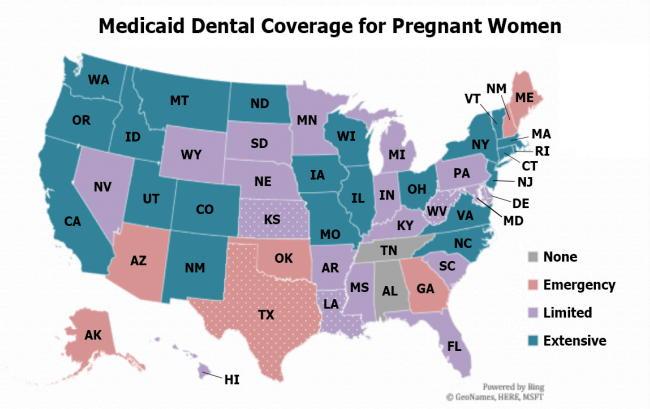
As previously discussed, teledentistry is an innovative strategy to increase access to dental care services. Currently, 49 states include Medicaid reimbursement for telemedicine programs (Center for Connected Health Policy, 2018). However, not all states include teledentistry as part of telemedicine programs. Nationally, dental coverage for pregnant women varies per state and therefore telehealth coverage is also affected (AZDHS, 2009). Few states offer teledentistry reimbursement through the state’s Medicaid program and it is often limited to “synchronous” (live video) interactions (ASTDD, 2019). Additionally, there are challenges with reimbursement as some insurances do not consider dental hygienists a part of teledentistry services as a rendering provider.
Arizona is one of the few states where teledentistry is recognized as a reimbursable service under telehealth through the Arizona Health Care Cost Containment System (AZDHS, 2009). While it is an innovative service to increase dental care access, there are financial barriers associated with its use. Costs to implement teledentistry may be expensive. Exact financial figures of teledentistry costs have not been reported. Teledentistry requires data management and imaging software compatible for synchronous interactions, digital oral cameras, radiographic equipment transferrable to digital images, and computer equipment. These equipment costs are vital to the operation of teledentistry and may be associated with surmounting financial costs.
Although dental care providers may oppose teledentistry due to startup costs to implement it, these costs may be alternatively considered as an investment. Benefits of teledentistry may reduce total billed claim costs. If hypothetically, a teledentist visit costs $50 and at least half of dental clinic members utilize the services, the overall claim may counterbalance fees associated with the digital service (Fontana & Wix, 2018).

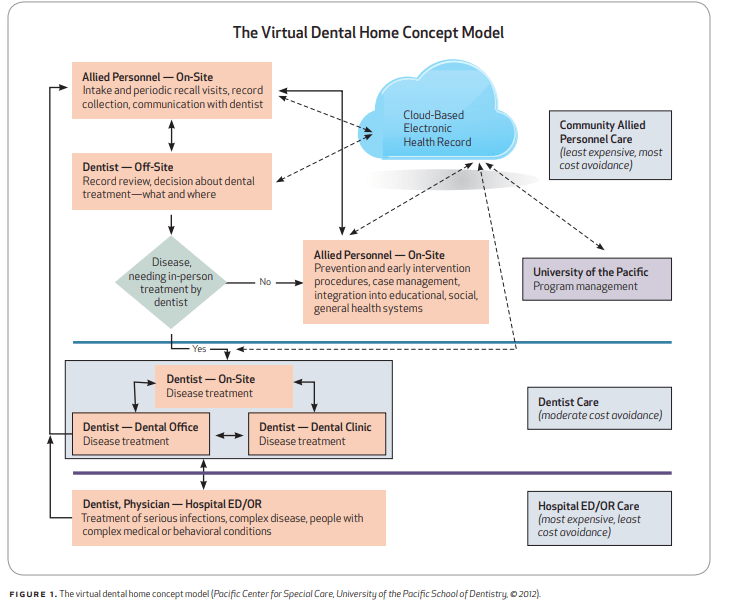
Teledentistry’s unique virtual capabilities may make it easier and more likely for patients to utilize these services especially in the context of preventive health. Increased participation in teledentistry may lead to better oral health outcomes and fewer higher cost services for advanced oral health treatment. California’s Virtual Dental Home is a great example of how teledentistry is cost-effective and can increase access to vulnerable populations. In dental care for children, VDH costs were approximately 40% less for diagnostic and preventive procedures compared to the state’s dental Medicaid program (Fontana& Wix, 2018). These same successful models can apply to pregnant women with teledentistry. The challenge in implementing this service for pregnant women would be stakeholder buy in from Medicaid insurance programs and dental care providers. However, it is necessary to look past profits for this service and work towards providing services that decrease gaps in health equity for pregnant women.
References
Arizona Department of Health Services. (2009). Teledentistry in Arizona. Retrieved from https://www.azdhs.gov/documents/prevention/womens-childrens-health/reports-fact-sheets/oral-health/teledentistry-arizona.pdf
Association of State & Territorial Dental Directors. (2019). Teledentistry: How technology can facilitate access to care [White paper]. Retrieved April 17, 2020, from Assosciation of State & Territorial Dental Directors: https://www.astdd.org/docs/teledentistry-how-technology-can-facilitate-access-to-care-3-4-19.pdf
Center for Connected Health Policy. (2018). State telehealth laws. Retrieved from https://www.cchpca.org/sites/default/files/2018-10/CCHP_50_State_Report_Fall_2018.pdf
Fontana, J., Wix, D. (2018). Value proposition of teledentistry: Cost savings, improved services, and more [White paper]. Retrieved April 17, 2020, from Milliman: https://careers.milliman.com/uploadedFiles/insight/2018/value-propostition-teledentistry.pdf